Dental Implants
Evaluating Your Professional Options for Care
Millions of people throughout the world now have a better quality of life because of dental implants. Dental implants are the only tooth replacement option that preserves bone and doesn't compromise the health of adjacent teeth — and they can potentially last a lifetime. Implants are today's preferred choice for restoring your natural smile with replacements that look, feel and function like natural teeth.
In Part One of our series we discussed the problems that follow tooth loss — the loss of alveolar (tooth-supporting) bone, changes to the face and jaws — and the subsequent impact on personal and social well-being. Maintaining alveolar bone is necessary for proper tooth replacement with dental implants, which are state of the art dentistry. We also considered other tooth replacement alternatives and why implants, long term, are the most cost effective.
In Part Two, we'll discuss the most suitable dental health professionals for both placing implants and fabricating the teeth that attach to them. We'll also give advice on where to go — and why, as well as when and how to make these important choices.
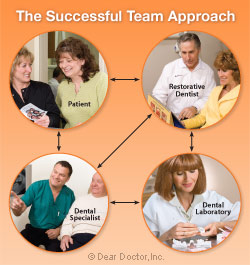 |
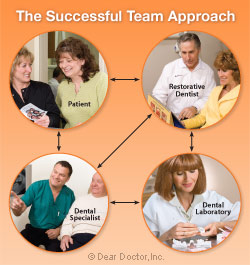
Figure 1: An experienced team understands what each member needs from the others and works in harmony to achieve health, proper function and a beautiful result.
Click to enlarge |
Choosing the Right Dental Team for Successful Implant Treatment
What are the advantages of a team approach? Think of it this way: an experienced dental team is like a well-rehearsed and experienced orchestra — though each individual knows his particular instrument well, when they all play together in harmony with the other members of the orchestra, the end result is beautiful music [Figure 1].
Implants are normally placed by dental surgical specialists (periodontists and oral surgeons) and in some cases general dentists who have undertaken special training in implantology and surgery. Implant placement requires planning and involves collaborative efforts between the surgeon (dental specialist), restorative dentist (general dentist or prosthodontist) and dental laboratory technician who is responsible for building the crowns on successfully integrated implants.
Most often your general dentist is the place to start. Some general dentists will have more knowledge than others in the field of implant dentistry depending on their individual interest, knowledge and expertise. The responsibility lays with the general dentist in communicating his/her expertise and comfort level and referring you to specialists so that together you can make confident decisions.
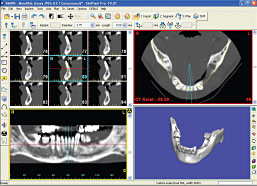 |
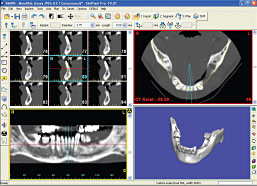
| Figure 2: CAT scan technology provides dentistry with images that allow for proper implant placement and safety. |
| Photo courtesy of Materialise Dental Inc. |
The following is a general sequence of steps necessary in planning dental implant treatment so that your dental team has all the facts they need for your situation. This includes an assessment of your medical status and general health — to determine your fitness for surgery — and an examination of your overall dental health, including;
- The site where the potential implant or implants are to be placed;
- Study models (molds) of your teeth to assess your bite;
- Photographs, especially if there is an aesthetic concern;
- Special radiographs (x-rays) to assess bone quantity and quality [Figure 2];
- Fabrication of surgical guides or templates to ensure accurate surgical implant placement.
This will provide answers to two critical questions necessary for successful implant treatment: Is there enough bone; and is it in the right place to allow tooth replacemen
Insufficient Bone — “Regeneration” In Our Generation
Sufficient bone volume for implant placement is vitally important to proper tooth placement resulting in both the most natural-looking and properly functioning tooth. Today there is general scientific agreement supporting the concept that when a tooth is removed a bone graft placed into the extraction site will minimize inevitable melting away of bone or “resorption.” Maintaining “bone volume” following removal of a tooth will facilitate implant placement in the best possible position.
Understanding the principles of wound healing now allows for regeneration of bone to occur using a variety of techniques. Most include opening the gingival (gum) tissues to expose the bone and then augmenting the existing or remaining bone by adding bone grafting materials to it. Healing of the bone can be enhanced by the utilization of membranes which cover the grafts and act like little subterranean band-aids to “guide bone regeneration.” Along with other biologically active molecules (found normally in the body) these techniques promote and enhance healing. In addition, excellent techniques exist for replacing and adding gingival gum tissues.
These surgical procedures are generally carried out by a periodontist or oral surgeon skilled and experienced in these techniques, especially in advanced situations. When creating new bone for implant placement, particularly in the upper jaw where sinuses are involved and bone grafting is necessary, these procedures are more predictably carried out in the hands of a specialist or a general dentist who has taken special and advanced training.
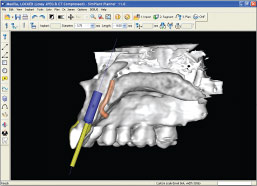 |
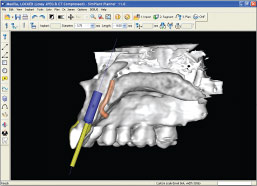
| Figure 3: Using CAT scan technology, a dentist can verify that there is sufficient bone to place an implant in the right location for an aesthetically pleasing crown. |
| Photo courtesy of Materialise Dental Inc. |
Implant Placement and Positioning
Sometimes described as “top down treatment planning,” the teeth to be replaced are recreated in a wax model form by a dental laboratory technician. The idea is then to establish the position of the underlying bone and to make sure the implant(s) is properly aligned (down) with the wax tooth form (top). The implant position can then be predetermined using a combination of specialized radiographs (x-rays) and imaging technology to assure success and in the process avoid major structures like nerves and air sinuses [Figure 3].
From this information surgical guides are made to assist the surgeon in precise implant placement; this in turn will assure the restorative dentist (general dentist or prosthodontist) that a crown will fit in the right position. If the bite will not accommodate implant placement, orthodontic treatment (braces carried out by an orthodontist) may be necessary to reposition teeth.
This process is analogous to the scuba diving adage, “Plan the dive and dive the plan.” A lot of preparatory work goes into initially deciding where an implant is going to be placed long before the actual surgery.
Finally, even with all the appropriate diagnosis and preparatory work, it's not a slam dunk — surgical know how does count. Surgical technique is in part an art, dependent upon proper knowledge, training and experience that can take years to acquire. It really comes down to this: every expert is an artist in his/her own field. Working on his/her particular canvas with all the appropriate information and experience at hand, the surgeon creates a work of art using materials with which he/she is most familiar.t with an implant?
Crown Manufacture and Placement
After the successful osseointegration (osseo – bone, integrate – join or fuse with) of the implant(s) to the jawbone your general dentist or prosthodontist (crown and bridge specialist), together with a skilled laboratory technician, will make a crown to fit on top of the implant that will precisely mimic a normal tooth both in form and function. Even this is not a simple task. It requires accurate record-taking and the transfer of this information to the dental laboratory for “abutment” fabrication (the part that fits into the implant and holds the crown in place). The crown of the tooth is then made of porcelain-like materials that look and function exactly like natural teeth. Implant success rates are extremely high and give patients many years of function and satisfaction.
Technical Challenges — Aesthetic Areas and “Teeth In A Day”
Achieving acceptable aesthetic results with implants is most challenging in highly visible areas like the front of the mouth, particularly in people who show not only teeth but the gum tissues as well. In these cases the whole tooth/gum tissue complex must be recreated including the papillae, the pink gum tissues that fill the triangular spaces between healthy teeth. It's at this point where knowledge and experience really come to the forefront.
There is a lot of advertising about “teeth in a day” where implant results can seemingly be achieved in a lot less time. In the right circumstances where multiple implants replace missing teeth, and where crowns (the portion of the teeth you see in the mouth) can be attached to them in such a way as to prevent any movement, “teeth in a day” is a possibility. This is accomplished by “splinting” the crowns to multiple implants — a precise fitting splint that keeps them movement free. However, this still requires multiple appointments for proper assessment, diagnosis and treatment-planning prior to “teeth in a day.” It also requires experience, great precision and care.
In some instances implants can be placed directly into extraction sockets and occasionally temporary crowns placed simultaneously. This also includes single tooth replacement, but stabilizing an implant in this situation is even more precarious and critical for success.
Our advice can be distilled to this: successful dental implant treatment can't be accomplished overnight and shouldn't be hurried. Anyone who is serious about dental implant treatment should first secure the services of well-trained and experienced dental professionals. Embracing this prudent route will greatly enhance the chances of a successful outcome.(Continued)